Understanding and Addressing Body Aches with ICD-10 Codes
Body aches, medically termed myalgia, are a common ailment experienced by individuals of all ages. These aches can range from mild discomfort to debilitating pain, significantly impacting daily life. When a patient presents with body aches, healthcare professionals rely on the International Classification of Diseases, Tenth Revision (ICD-10) coding system to document the condition accurately. This guide provides an in-depth exploration of ICD-10 codes related to body aches, helping both healthcare providers and individuals understand the diagnostic process and potential underlying causes.
This comprehensive resource aims to provide clarity on the use of ICD-10 codes for body aches, offering insights into potential diagnoses, treatment strategies, and preventative measures. We will delve into the nuances of coding, exploring various related conditions and their corresponding codes, ultimately empowering you with a deeper understanding of this prevalent health concern. Our goal is to equip you with the knowledge necessary to navigate the complexities of diagnosis and treatment effectively.
Navigating the ICD-10 Landscape for Myalgia
The ICD-10 coding system is a standardized diagnostic tool used worldwide to classify and code diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. In the context of body aches, ICD-10 provides specific codes that help healthcare providers document the patient’s condition, track its progression, and facilitate appropriate billing and insurance claims. The specific code chosen depends on various factors, including the location, severity, and underlying cause of the body aches.
Several ICD-10 codes may be relevant when documenting body aches. While there isn’t a single, all-encompassing code for “body aches,” healthcare professionals typically use codes that reflect the underlying condition causing the pain. For instance, if body aches are a symptom of influenza, the appropriate ICD-10 code for influenza would be used. Similarly, if the aches are due to fibromyalgia, the code for fibromyalgia would be assigned. Understanding these nuances is crucial for accurate diagnosis and effective treatment.
The ICD-10-CM (Clinical Modification) is used in the United States. It is based on the World Health Organization’s ICD-10, but it has been expanded to provide more specificity for diagnostic and morbidity coding.
Common ICD-10 Codes Associated with Body Aches
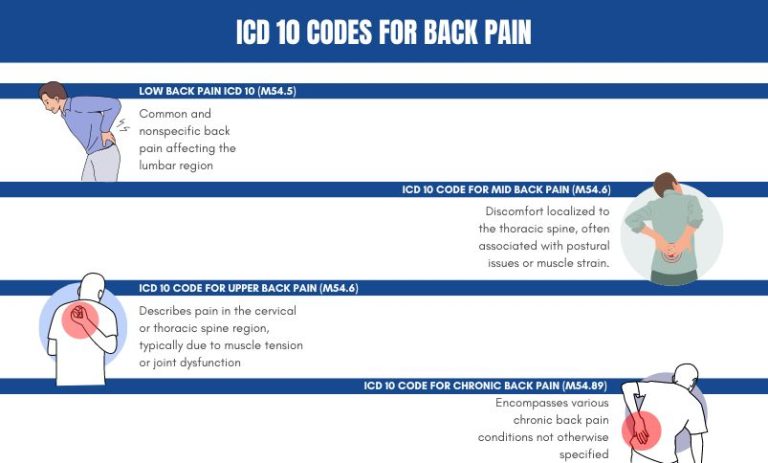
Here are some of the most frequently used ICD-10 codes when documenting body aches, along with their corresponding conditions:
- M79.1: Myalgia – This is a general code for muscle pain. It is often used when the specific cause of the body aches is not yet known or when the pain is widespread.
- M54.9: Dorsalgia, unspecified – This code is used for back pain when a more specific diagnosis hasn’t been made.
- M25.50: Pain in unspecified joint – Used when the pain is located in a joint, but the specific joint is not specified.
- M79.7: Fibromyalgia – This code is used for fibromyalgia, a chronic condition characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory and mood issues.
- R50.9: Fever, unspecified – Body aches are a common symptom of fever. If fever is present, this code may be used in conjunction with a code for the underlying cause of the fever.
- J10-J11: Influenza – These codes are used for influenza (flu). Body aches are a hallmark symptom of the flu, so these codes are frequently used during flu season. The specific code depends on whether the influenza virus is identified.
- B97.29: Other coronavirus as the cause of diseases classified elsewhere – This code gained prominence during the COVID-19 pandemic. Body aches are a common symptom of COVID-19, and this code is used to indicate that the coronavirus is the underlying cause of the aches.
- M54.5: Low back pain – This code is specifically for pain in the lower back.
- M25.561: Pain in right knee – Used when pain is specifically located in the right knee.
- M25.562: Pain in left knee – Used when pain is specifically located in the left knee.
The Role of Accurate Coding
Accurate coding is paramount for several reasons. First, it ensures that patients receive appropriate and timely medical care. By accurately documenting the patient’s condition, healthcare providers can develop effective treatment plans tailored to their specific needs. Second, accurate coding is essential for proper billing and insurance reimbursement. Insurance companies rely on ICD-10 codes to process claims and determine coverage. Incorrect coding can lead to claim denials or delays in payment. Finally, accurate coding is vital for public health tracking and research. By collecting and analyzing data on diseases and conditions, public health officials can identify trends, monitor outbreaks, and develop strategies to improve population health.
Unraveling the Underlying Causes of Body Aches
Body aches can stem from a myriad of underlying causes, ranging from common viral infections to chronic musculoskeletal conditions. Identifying the root cause is crucial for effective treatment and management. Here are some of the most common culprits behind body aches:
- Viral Infections: Infections like the flu, common cold, and COVID-19 are notorious for causing widespread body aches. These aches are often accompanied by other symptoms such as fever, cough, and fatigue.
- Muscle Strain or Injury: Overexertion, trauma, or repetitive motions can lead to muscle strains or injuries, resulting in localized or widespread body aches.
- Arthritis: Various forms of arthritis, including osteoarthritis and rheumatoid arthritis, can cause joint pain and stiffness, often accompanied by muscle aches and fatigue.
- Fibromyalgia: This chronic condition is characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and mood issues.
- Dehydration: Insufficient fluid intake can lead to muscle cramps and aches.
- Electrolyte Imbalance: Imbalances in electrolytes such as potassium, sodium, and calcium can disrupt muscle function and cause aches.
- Autoimmune Diseases: Conditions like lupus and multiple sclerosis can trigger inflammation and pain throughout the body.
- Medications: Certain medications, such as statins and chemotherapy drugs, can cause muscle aches as a side effect.
- Stress and Anxiety: Psychological stress and anxiety can manifest as physical symptoms, including muscle tension and body aches.
It’s important to consult with a healthcare professional to determine the underlying cause of your body aches and receive appropriate treatment.
The Diagnostic Process: Pinpointing the Cause of Your Aches
When you visit a healthcare provider for body aches, they will typically conduct a thorough evaluation to determine the underlying cause. This evaluation may include:
- Medical History: Your doctor will ask about your past medical conditions, medications, allergies, and family history.
- Physical Examination: Your doctor will perform a physical exam to assess your range of motion, muscle strength, and reflexes. They may also palpate (feel) your muscles and joints to identify areas of tenderness or inflammation.
- Symptom Assessment: Your doctor will ask detailed questions about your symptoms, including the location, severity, duration, and triggers of your body aches.
- Diagnostic Tests: Depending on your symptoms and medical history, your doctor may order diagnostic tests such as blood tests, X-rays, or MRIs to help identify the underlying cause of your body aches.
Based on the results of these evaluations, your doctor will be able to make an accurate diagnosis and develop a personalized treatment plan.
Leading Pain Relief Options for Body Aches
While addressing the underlying cause of body aches is crucial, managing the pain itself is also important for improving quality of life. Several pain relief options are available, ranging from over-the-counter medications to prescription therapies and alternative treatments.
- Over-the-Counter Pain Relievers: Medications like acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) and naproxen (Aleve) can effectively relieve mild to moderate body aches.
- Prescription Pain Medications: For more severe pain, your doctor may prescribe stronger pain medications such as opioids or muscle relaxants. However, these medications should be used with caution due to their potential for side effects and addiction.
- Topical Pain Relievers: Creams, gels, and patches containing ingredients like menthol, capsaicin, or lidocaine can provide localized pain relief.
- Physical Therapy: Physical therapy can help improve muscle strength, flexibility, and range of motion, reducing pain and preventing future injuries.
- Alternative Therapies: Some people find relief from body aches through alternative therapies such as acupuncture, massage therapy, chiropractic care, and yoga.
It’s important to discuss your pain relief options with your doctor to determine the most appropriate approach for your specific condition.
Key Features of Effective Pain Management Strategies
Effective pain management goes beyond simply masking the symptoms. It involves a holistic approach that addresses the underlying cause of the pain, reduces inflammation, improves muscle function, and enhances overall well-being. Here are some key features of effective pain management strategies:
- Personalized Treatment Plans: Every individual experiences pain differently, so treatment plans should be tailored to their specific needs and preferences.
- Multimodal Approach: Combining different pain relief modalities, such as medication, physical therapy, and alternative therapies, can often provide better results than relying on a single approach.
- Focus on Function: The goal of pain management should be to improve the patient’s ability to perform daily activities and participate in social and recreational activities.
- Patient Education: Empowering patients with knowledge about their condition and treatment options can help them take an active role in their care.
- Long-Term Management: Chronic pain often requires ongoing management to prevent flare-ups and maintain quality of life.
Significant Advantages of a Holistic Pain Management Approach
A holistic approach to pain management offers several significant advantages over traditional methods that focus solely on medication. By addressing the physical, psychological, and social aspects of pain, holistic pain management can lead to:
- Reduced Reliance on Medications: By incorporating non-pharmacological therapies, patients can often reduce their reliance on pain medications, minimizing the risk of side effects and addiction.
- Improved Function and Mobility: Physical therapy, exercise, and other rehabilitation techniques can help improve muscle strength, flexibility, and range of motion, allowing patients to perform daily activities more easily.
- Enhanced Mood and Mental Well-being: Chronic pain can often lead to depression, anxiety, and other mental health issues. Holistic pain management addresses these psychological aspects of pain, improving mood and overall well-being.
- Better Sleep Quality: Pain can disrupt sleep, leading to fatigue and reduced quality of life. Holistic pain management techniques such as relaxation exercises and sleep hygiene can help improve sleep quality.
- Increased Patient Satisfaction: Patients who receive holistic pain management often report higher levels of satisfaction with their care and improved quality of life.
The Value of Seeking Expert Guidance
Navigating the complexities of body aches and pain management can be challenging. Seeking guidance from healthcare professionals who specialize in pain management can provide numerous benefits, including:
- Accurate Diagnosis: Pain specialists have the expertise to accurately diagnose the underlying cause of your body aches, ensuring that you receive appropriate treatment.
- Personalized Treatment Plans: Pain specialists can develop personalized treatment plans tailored to your specific needs and preferences, taking into account your medical history, symptoms, and lifestyle.
- Access to Advanced Therapies: Pain specialists have access to a wide range of advanced therapies, including interventional pain procedures, that may not be available from other healthcare providers.
- Coordination of Care: Pain specialists can coordinate your care with other healthcare professionals, such as physical therapists, psychologists, and surgeons, to ensure that you receive comprehensive and integrated care.
- Improved Outcomes: Studies have shown that patients who receive care from pain specialists often experience better outcomes, including reduced pain, improved function, and enhanced quality of life.
Preventative Strategies: Minimizing Your Risk of Body Aches
While not all body aches are preventable, there are several strategies you can implement to minimize your risk:
- Maintain a Healthy Lifestyle: Regular exercise, a balanced diet, and adequate sleep can help strengthen your muscles and immune system, reducing your risk of injury and illness.
- Practice Good Posture: Maintaining good posture can help prevent muscle strain and back pain.
- Stay Hydrated: Drinking plenty of water can help prevent muscle cramps and aches.
- Manage Stress: Stress can contribute to muscle tension and body aches. Practice relaxation techniques such as yoga, meditation, or deep breathing exercises to manage stress.
- Warm Up Before Exercise: Warming up before exercise can help prepare your muscles for activity, reducing your risk of injury.
- Avoid Overexertion: Gradually increase the intensity and duration of your workouts to avoid overexertion and muscle strain.
- Get Vaccinated: Vaccinations can help protect you from viral infections that can cause body aches.
Final Thoughts: Taking Control of Your Well-being
Understanding the role of ICD-10 codes in diagnosing and managing body aches is essential for both healthcare providers and individuals seeking relief. By accurately documenting the condition and identifying the underlying cause, healthcare professionals can develop effective treatment plans tailored to each patient’s specific needs. Remember, while this guide provides valuable information, it is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment of any medical condition.
If you’re experiencing persistent or severe body aches, consider seeking expert guidance from a pain management specialist. They can provide a comprehensive evaluation, personalized treatment plan, and ongoing support to help you regain control of your well-being. Share your experiences with managing body aches in the comments below and help others find effective solutions.
